- Home
- MetroHealth Research Institute
- Research News
- 2019 Featured Stories
2019 Featured Stories
12/09/19 Rep. Crossman Tours MetroHealth, Meets with Rehab Institute Staff
 Several members of the MetroHealth Rehabilitation Institute team had an opportunity Friday to showcase their work and our facilities to State Rep. Jeff Crossman, who represents Parma, Brooklyn Heights, Cuyahoga Heights, and part of southwest Cleveland.
Several members of the MetroHealth Rehabilitation Institute team had an opportunity Friday to showcase their work and our facilities to State Rep. Jeff Crossman, who represents Parma, Brooklyn Heights, Cuyahoga Heights, and part of southwest Cleveland.
John Chae, MD, Vice President of Research and Sponsored Programs and Chair of the Department of Physical Medicine and Rehabilitation (PM&R); P. Hunter Peckham, PhD, Co-Director of the MetroHealth Rehabilitation Institute and a staff scientist in Orthopedics and PM&R; Jayme Knutson, PhD, Director of Research for PM&R; and Kim Anderson, PhD, a staff scientist in PM&R, hosted the tour.
Rep. Crossman had an opportunity to learn about the research and work being done at the Rehabilitation Institute, especially in the areas of spinal cord injury, stroke therapies and technology to relieve chronic pain. The Institute focuses on restoring function, social participation and quality of life to persons with significant disabilities. The team’s approach is to deliver outstanding rehabilitation care, train the next generation of rehabilitation clinicians and scientists, and discover new knowledge that becomes part of our standard of care. Rep. Crossman also toured The Zubizarreta House, our fully accessible facility where out-of-town patients can stay when receiving these treatments at MetroHealth. The 7,000-square-foot, one-story house can house several patients and is located near the MetroHealth Old Brooklyn Medical Center.
11/22/19 Kavita Arora, MD, Appointed CWRU-MetroHealth Dierker-Biscotti Women’s Wellness Endowed Professor

Dr. Arora completed Medical School at Jefferson Medical College and received a Master’s Degree in Bioethics at the University of Pennsylvania. She joined the Department of Obstetrics & Gynecology with a secondary appointment in the Department of Bioethics, after completing her residency in Obstetrics & Gynecology at Northwestern University’s Feinberg School of Medicine in 2013. Since joining our faculty Dr. Arora has provided women’s health services to our patients at MetroHealth, and to active duty service members and veterans at the Louis Stokes Cleveland Veterans Affairs Medical Center.
Dr. Arora’s research is focused on understanding and eradicating the disparities in access and autonomy afforded to vulnerable women regarding long-acting reversible contraception and permanent sterilization. She combines her expertise in theoretical bioethics, qualitative and quantitative research methodologies, and understanding of health policy to further this mission. Funded through the NIH-CWRU KL2 scholars program, the CWRU Social Justice Institute, the Society for Family Planning, HRSA, and the NIH-funded CWRU Center for Genetics Research, Ethics and the Law, Dr Arora’s research has resulted in over 50 peer-reviewed manuscripts in major national and international journals, including; The American Journal of Public Health, American Journal of Bioethics, Journal of Medical Ethics, Obstetrics and Gynecology, and the American Journal of Obstetrics and Gynecology.
Dr. Arora has served on committees of key national organizations that have the potential to impact women’s health and bioethics, including; the American Medical Association, the American College of Obstetricians and Gynecologists, and the American Society for Bioethics and Humanities. She currently serves on the American Society for Bioethics and Humanities Board of Directors. Locally, Dr. Arora serves as Director of Quality for the Department of Obstetrics & Gynecology at MetroHealth, and as unit leader for Reproductive Ethics in the Masters of Bioethics program at Case Western Reserve University. She is a recognized teacher and mentor, serving as faculty advisor and research mentor for numerous Case Western Reserve University Medical Students, ObGyn Residents, Master’s of Public Health and Bioethics candidates. Her excellence in teaching has been recognized every year between 2010 and 2018. In 2014, Dr. Arora was recognized with the CREOG National Faculty Award for Excellence in Resident Teaching.
As the Dierker-Biscotti Women’s Wellness Professor, Dr. Arora will continue to serve as a tribute to the lifelong contributions and efforts of Drs. LeRoy Dierker and Matthew Biscotti to improve women’s health and wellness.
10/08/19 Dennis Bourbeau, PhD, Receives $735,000 Craig H. Neilson Award to Improve Bladder Function for Patients with Spinal Cord Injury
 Dennis Bourbeau, PhD, Staff Scientist in the department of Physical Medicine and Rehabilitation (PM&R), received a 3-yr, $735,000 grant from the Craig H. Neilsen Foundation entitled “Ambulatory closed-loop stimulation to inhibit neurogenic bladder overactivity”.
Dennis Bourbeau, PhD, Staff Scientist in the department of Physical Medicine and Rehabilitation (PM&R), received a 3-yr, $735,000 grant from the Craig H. Neilsen Foundation entitled “Ambulatory closed-loop stimulation to inhibit neurogenic bladder overactivity”.
Following spinal cord injury (SCI), most individuals develop neurogenic bladder characterized by overactivity, which can severely impair a person’s health and quality of life and is associated with high costs. Electrical stimulation of the genital nerves has been shown to inhibit overactive bladder to improve bladder capacity and urinary continence in men and women with SCI. The objective of this project is to evaluate the potential feasibility and effectiveness of automated closed-loop genital nerve stimulation to stop unwanted bladder contractions using a custom algorithm and a wireless, catheter-free bladder pressure sensor developed with collaborators.
Dr. Bourbeau is Assistant Professor of PM&R at Case Western Reserve University.
09/30/19 P. Hunter Peckham, PhD, elected Fellow of the International Academy of Medical and Biological Engineering
 P. Hunter Peckham, PhD, Co-Director of the MetroHealth Rehabilitation Institute and staff scientist in the Departments of Orthopedics and Physical Medicine and Rehabilitation (PM&R), was elected Fellow of the International Academy of Medical and Biological Engineering (IAMBE). IAMBE is a non-profit society of distinguished scholars engaged in medical and biological engineering research to further the field of biomedical engineering or bioengineering. The Academy is composed of Fellows who have made significant contributions to and played leadership roles in the field of medical and biological engineering. This honor recognizes Dr. Peckham’s contributions to and leadership in the field of medical and biological engineering at the international level.
P. Hunter Peckham, PhD, Co-Director of the MetroHealth Rehabilitation Institute and staff scientist in the Departments of Orthopedics and Physical Medicine and Rehabilitation (PM&R), was elected Fellow of the International Academy of Medical and Biological Engineering (IAMBE). IAMBE is a non-profit society of distinguished scholars engaged in medical and biological engineering research to further the field of biomedical engineering or bioengineering. The Academy is composed of Fellows who have made significant contributions to and played leadership roles in the field of medical and biological engineering. This honor recognizes Dr. Peckham’s contributions to and leadership in the field of medical and biological engineering at the international level.
Dr. Peckham is Member of the National Academy of Engineering, Fellow of the National Academy of Inventors and Fellow of the American Institute for Medical and Biological Engineering. Dr. Peckham is Distinguished University Professor, Donnell Professor of Biomedical Engineering and Professor of Orthopedics and Physical Medicine and Rehabilitation at Case Western Reserve University.
09/26/19 Shari Bolen, MD, Participates in Hypertension Control Meeting Sponsored by the Centers for Disease Control and Prevention
 Shari Bolen MD, MPH, Associate Division Director of Internal Medicine and faculty member in the Center for Healthcare Research and Policy, served as an invited participant in a Hypertension Control Meeting sponsored by the Centers for Disease Control and Prevention (CDC) Sept 9-10, 2019. The invitation was based on her CDC-funded work with MetroHealth and other regional practice sites to improve blood pressure control.
Shari Bolen MD, MPH, Associate Division Director of Internal Medicine and faculty member in the Center for Healthcare Research and Policy, served as an invited participant in a Hypertension Control Meeting sponsored by the Centers for Disease Control and Prevention (CDC) Sept 9-10, 2019. The invitation was based on her CDC-funded work with MetroHealth and other regional practice sites to improve blood pressure control.
The CDC convened health care and public health professionals and organizations, national and community-based organizations, academicians, employers, payers and philanthropic organizations to plan action steps for drastically improving national hypertension control rates. The goal of the meeting was to develop a national action plan to move the current hypertension control rate to 80% by 2022.
Dr. Bolen is Associate Professor of Medicine at the Case Western Reserve University School of Medicine.
09/16/19 John Chae, MD, is co-editor of a major textbook in Physical Medicine and Rehabilitation
 John Chae, MD, VP for Research and Sponsored Programs and Chair of the Department of Physical Medicine and Rehabilitation (PM&R), is co-editor of DeLisa’s Physical Medicine and Rehabilitation: Principles and Practice. The 1,760-page volume presents the most comprehensive review of the state of the art, evidence-based clinical recommendations for physiatric management of disorders affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles and tendons.
John Chae, MD, VP for Research and Sponsored Programs and Chair of the Department of Physical Medicine and Rehabilitation (PM&R), is co-editor of DeLisa’s Physical Medicine and Rehabilitation: Principles and Practice. The 1,760-page volume presents the most comprehensive review of the state of the art, evidence-based clinical recommendations for physiatric management of disorders affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles and tendons.
Written by the most recognized names in PM&R research and education, the sixth edition of DeLisa’s pioneering textbook presents both the scientific fundamentals as well as the latest clinical treatments and rehabilitative techniques for a broad array of conditions, disabilities and diseases. Other PM&R faculty at the MetroHealth System contributing to the volume include Jayme Knutson, PhD, Director of Research and Associate Professor of PM&R and Richard Wilson, MD, Director of Division of Neurological Rehabilitation and Associate Professor of PM&R. Dr. Chae is Professor and Chair of PM&R and Professor of Biomedical Engineering.
08/13/19 Charles Bark, MD, receives $7.2 million NIH grant to study transmission of tuberculosis in Uganda

08/02/19 Dr. Laurita receives $2.8 million NIH award to develop optically guided catheter ablation for atrial fibrillation
 Kenneth Laurita, PhD, scientific staff in the Heart and Vascular Center was awarded a 4-year, $2,800,000 NIH grant to develop optically guided catheter ablation of atrial fibrillation. Atrial fibrillation affects approximately 3 million patients and its prevalence is expected to rise as the population ages. Catheter ablation, the preferred treatment strategy for symptomatic patients, currently has several limitations that can account for atrial fibrillation recurrence in many patients. We propose that optically guided ablation using optical coherence tomography and near-infrared spectroscopy can overcome these limitations and, ultimately, improve atrial fibrillation ablation outcomes.
Kenneth Laurita, PhD, scientific staff in the Heart and Vascular Center was awarded a 4-year, $2,800,000 NIH grant to develop optically guided catheter ablation of atrial fibrillation. Atrial fibrillation affects approximately 3 million patients and its prevalence is expected to rise as the population ages. Catheter ablation, the preferred treatment strategy for symptomatic patients, currently has several limitations that can account for atrial fibrillation recurrence in many patients. We propose that optically guided ablation using optical coherence tomography and near-infrared spectroscopy can overcome these limitations and, ultimately, improve atrial fibrillation ablation outcomes.
Dr. Laurita’s clinician partner and co-investigator (Co-I) at the MetroHealth System is Ohad Ziv, MD, attending physician in the Heart and Vascular Center. MetroHealth, in a multi-Principal Investigator (PI) collaboration with Dr. Andrew Rollins at Case Western Reserve University (CWRU) and Dr. Christine P. Hendon at Columbia University, is in a unique position to revolutionize the treatment of atrial fibrillation.
Dr. Laurita (PI) is an Associate Professor of Medicine (Cardiology) and Biomedical Engineering, and Dr. Ziv (Co-I) is an Assistant Professor of Medicine (Cardiology), CWRU.
07/20/19 MetroHealth part of study showing home-based telerehabilitation is as effective as in-clinic therapy in stroke patients
 MetroHealth served as a major contributor to a multi-center, randomized, controlled trial that demonstrated home-based telerehabilitation was as effective as in-clinic therapy for upper limb recovery after stroke. The paper entitled “Efficacy of Home-Based Telerehabilitation vs In-Clinic Therapy for Adults After Stroke” was published in the June, 2019 issue of JAMA Neurology.
MetroHealth served as a major contributor to a multi-center, randomized, controlled trial that demonstrated home-based telerehabilitation was as effective as in-clinic therapy for upper limb recovery after stroke. The paper entitled “Efficacy of Home-Based Telerehabilitation vs In-Clinic Therapy for Adults After Stroke” was published in the June, 2019 issue of JAMA Neurology.
One hundred twenty-four participants who experienced a stroke 4 to 36-weeks prior and had mild to moderate upper limb deficits were enrolled at 11 sites across the United States between 9/18/15 and 12/28/17. Both groups received supervised and unsupervised treatment sessions that focused on repetitive task practice and functional training over a 6-week period.
Unsupervised sessions for both groups were carried out at home. For the supervised sessions, the TR group received their treatments at home using an internet-enabled computer and 12 gaming input devices with remote therapist supervision via video conferencing. The IC group received their supervised sessions in clinic under the “in-person” supervision of a therapist.
At 30 days after the end of treatment, both groups had experienced similar improvements in their upper limb hemiparesis and function based on objective measures, indicating that TR is not inferior to IC therapy. However, participant motivational factors and self-reported perception of motor and functional recovery were slightly higher in the IC group.
As the US healthcare system transitions to population health, telemedicine in general, and telerehabilitation in physical medicine and rehabilitation (PM&R) in particular, will be major considerations in the ongoing dialogue and formulation of value-based medicine.
Steven Cramer, MD, Professor of Neurology at the University of California, Irvine, served as the principal investigator (PI) of this NIH sponsored clinical trial. Jayme Knutson, PhD, Director of Research for the department of PM&R and Associate Professor of PM&R at Case Western Reserve University (CWRU), served as the site PI at MetroHealth. Among 11 sites, MetroHealth contributed the 3rd highest number of participants to the clinical trial. Other contributors to the trial at MetroHealth include Margaret M. Maloney, RN; Gregory Naples, MS; Amy S. Friedl, MS, OTR/L; Kristine M. Hansen, MPT; Mary Y. Harley, OT/L; Terri Z. Hisel, OTR/L; and John Chae, MD. In addition, MetroHealth was supported by the Cleveland NINDS Stroke Trial Collaborative (NIH U10 grant awarded to CWRU; PI: Anthony Furlan, MD).
07/15/19 Dr. Sehgal awarded $2.2 million NIH grant for community-based clinical trial on the efficacy of massage therapy after breast cancer surgery
 Ashwini Sehgal, MD, Director of the Center for Reducing Health Disparities (CRHD), was awarded a 4-yr, $2.2 million NIH R01 grant to evaluate the efficacy of massage therapy to reduce pain and immobility following breast cancer surgery. About 25-50% of women who undergo breast cancer surgery develop persistent chest wall pain and shoulder mobility limitations following surgery. Myofascial massage, a treatment technique that provides deep tissue massage with focus on muscles as well as the connective tissue that surrounds muscles, bones, and ligaments, may be effective in reducing post-mastectomy pain and immobility.
Ashwini Sehgal, MD, Director of the Center for Reducing Health Disparities (CRHD), was awarded a 4-yr, $2.2 million NIH R01 grant to evaluate the efficacy of massage therapy to reduce pain and immobility following breast cancer surgery. About 25-50% of women who undergo breast cancer surgery develop persistent chest wall pain and shoulder mobility limitations following surgery. Myofascial massage, a treatment technique that provides deep tissue massage with focus on muscles as well as the connective tissue that surrounds muscles, bones, and ligaments, may be effective in reducing post-mastectomy pain and immobility.
The grant will support a community-based, randomized controlled trial involving 202 women with persistent pain and mobility limitations. Participants in each group will receive 30 minutes of treatment twice weekly for 2 months. The treatment group will receive massage therapy while the control group will receive light touch therapy. Primary analyses will determine the impact of myofascial massage on pain and mobility limitations. Secondary analyses will examine the impact of myofascial massage on a number of secondary outcomes, including range of motion, quality of life, sleep, and body image.
Dr. Sehgal is the Duncan Neuhauser Professor of Community Health Improvement and Professor of Medicine, Bioethics and Population and Quantitative Health Services at Case Western Reserve University (CWRU). Co-investigators on the grant are Richard Wilson, MD, Director of the Division of Neurological Rehabilitation at the MetroHealth System and Associate Professor of Physical Medicine and Rehabilitation at CWRU; Jacquie Dolata, MBA, Research Manager, CRHD; and Jeff Albert, PhD, Professor of Population and Quantitative Health Sciences and Medicine at CWRU.
07/08/19 Kim Anderson, PhD, Receives $803,000 Department of Defense Grant to Study Recovery After Spinal Cord Injury and Community Re-entry
 Dr. Kim Anderson, a staff scientist in the Department of Physical Medicine and Rehabilitation (PM&R), was awarded a 3-year, $803,000 grant by the Department of Defense (DoD). Funds will be used to lead a qualitative research study to understand how veterans and civilians with spinal cord injury (SCI) experience recovery in their first year after injury as they attempt to reintegrate into the community.
Dr. Kim Anderson, a staff scientist in the Department of Physical Medicine and Rehabilitation (PM&R), was awarded a 3-year, $803,000 grant by the Department of Defense (DoD). Funds will be used to lead a qualitative research study to understand how veterans and civilians with spinal cord injury (SCI) experience recovery in their first year after injury as they attempt to reintegrate into the community.
Data will be collected by interviewing veterans and civilians living with SCI and their caregivers. Understanding the experience of veterans and civilians as they undergo recovery and navigate resources will offer clinicians and researchers opportunities to improve access and develop more relevant treatments to improve function and reintegration.
This study is a collaboration between researchers at the MetroHealth System, (Kim Anderson, PhD; Anne Bryden, MA, OTR/L); sociologists at Case Western Reserve University (Sue Hinze, PhD; Brian Gran, PhD) and clinicians at the Veterans Affairs Northeast Ohio Health System (Mary Ann Richmond, MD; Angela Kuemmel, PhD). Dr. Anderson joined the PM&R department in March of 2018 from the University of Miami where she was Professor of Neurological Surgery. Her appointment to Professor of PM&R is pending CWRU review.
05/17/19 Dr. Chae appointed to serve on the National Academy of Medicine Membership Subcommitee on Health and Technology
 John Chae, MD, Vice President for Research and Sponsored Programs and Chair of Physical Medicine and Rehabilitation, was appointed to serve on the National Academy of Medicine (NAM) Membership Subcommitee on Health and Technology. The NAM, formerly the Institute of Medicine, is one of three academies that make up the National Academies of Sciences, Engineering, and Medicine. Its mission is to improve health for all by advancing science, accelerating health equity, and providing independent, authoritative, and trusted advice nationally and globally. Seventy-five regular and 10 international members are elected annually by the membership “for distinguished contributions to medicine and health."
John Chae, MD, Vice President for Research and Sponsored Programs and Chair of Physical Medicine and Rehabilitation, was appointed to serve on the National Academy of Medicine (NAM) Membership Subcommitee on Health and Technology. The NAM, formerly the Institute of Medicine, is one of three academies that make up the National Academies of Sciences, Engineering, and Medicine. Its mission is to improve health for all by advancing science, accelerating health equity, and providing independent, authoritative, and trusted advice nationally and globally. Seventy-five regular and 10 international members are elected annually by the membership “for distinguished contributions to medicine and health."
For 2019, five slots will be allocated to the subject emphasis area of Health and Technology. The subcommittee will identify candidates with expertise in areas that include basic science and its translation to technologies that enhance health and patient care; engineering research and its translation to the development of instrumentation to support diagnosis, monitoring and other health-related activities; the curation of health data to allow inference; and the development and implementation of analytical methods leading to tools that can facilitate health-related assessments and decision-making to a wide range of users.
The National Academy of Sciences, the first of the three academies, was established in 1863 by an Act of Congress, signed by President Lincoln, as a private, nongovernmental institution to advise the nation on issues related to science and technology. The National Academies of Engineering and Medicine were established in 1964 and 1970, respectively. Dr. Chae is a member of the NAM and Professor and Chair of Physical Medicine and Rehabilitation and Professor of Biomedical Engineering at Case Western Reserve University.
05/16/19 Dr. Sossey-Alaoui Awarded $1.8 Million from the NIH NIH to Study Aggressive Form of Breast Cancer that Disproportionately Affects African American Women
 Khalid Sossey-Alaoui, PhD, staff scientist in the Division of Cancer Biology of the Department of Medicine, was awarded a $1.8 million grant from the National Cancer Institute (NCI) to study an aggressive form of breast cancer that disproportionately affects African American women. These “triple-negative breast cancers” or TNBCs are an unusually aggressive and metastatic subtype of breast cancer that also exhibit rapid rates of recurrence. Thus, TNBC patients have a poor prognosis as compared to individuals harboring non-TNBC tumors. Dr. Sossey-Alaoui’s group previously established WAVE3 (W3), a protein that regulates cell morphology and movement, as a novel promoter of TNBC development and metastatic progression. This R01 grant from the NCI will not only provide novel mechanistic insights into how W3 promotes TNBC metastasis, but will also deliver two major clinically relevant advancements by (a) establishing W3 as a major player in the maintenance of Cancer Stem Cells in TNBCs, and (b) administering W3 inhibitors in combination with chemotherapy as a novel treatment against TNBCs. Dr. Sossey-Alaoui is Assistant Professor of Medicine at the Case Western Reserve University School of Medicine.
Khalid Sossey-Alaoui, PhD, staff scientist in the Division of Cancer Biology of the Department of Medicine, was awarded a $1.8 million grant from the National Cancer Institute (NCI) to study an aggressive form of breast cancer that disproportionately affects African American women. These “triple-negative breast cancers” or TNBCs are an unusually aggressive and metastatic subtype of breast cancer that also exhibit rapid rates of recurrence. Thus, TNBC patients have a poor prognosis as compared to individuals harboring non-TNBC tumors. Dr. Sossey-Alaoui’s group previously established WAVE3 (W3), a protein that regulates cell morphology and movement, as a novel promoter of TNBC development and metastatic progression. This R01 grant from the NCI will not only provide novel mechanistic insights into how W3 promotes TNBC metastasis, but will also deliver two major clinically relevant advancements by (a) establishing W3 as a major player in the maintenance of Cancer Stem Cells in TNBCs, and (b) administering W3 inhibitors in combination with chemotherapy as a novel treatment against TNBCs. Dr. Sossey-Alaoui is Assistant Professor of Medicine at the Case Western Reserve University School of Medicine.
04/25/19 Dr. Kilgore awarded $600,000 grant from the Neilsen Foundation to study blood pressure monitoring during autonomic dysreflexia in spinal cord injury
 Kevin Kilgore, PhD, staff scientist in the departments of Orthopedics and Physical Medicine and Rehabilitation (PM&R), was awarded a $600,000, 3-year grant from the Craig H. Neilsen Foundation to develop an implanted blood pressure (BP) sensor for persons with spinal cord injury (SCI). The sensor will monitor BP during episodes of autonomic dysreflexia (AD), a lifelong and potentially life-threatening condition for individuals with SCI associated with a rapid rise in BP. The application proposes to estimate BP using implanted optical and electrical sensors and includes pre-clinical and clinical feasibility studies. The study will inform future design of a fully implanted version of the BP warning system. Although the first clinical target is AD for persons with SCI, Dr. Kilgore and his team plan to expand the use of this sensor to many other health monitoring applications in the future.
Kevin Kilgore, PhD, staff scientist in the departments of Orthopedics and Physical Medicine and Rehabilitation (PM&R), was awarded a $600,000, 3-year grant from the Craig H. Neilsen Foundation to develop an implanted blood pressure (BP) sensor for persons with spinal cord injury (SCI). The sensor will monitor BP during episodes of autonomic dysreflexia (AD), a lifelong and potentially life-threatening condition for individuals with SCI associated with a rapid rise in BP. The application proposes to estimate BP using implanted optical and electrical sensors and includes pre-clinical and clinical feasibility studies. The study will inform future design of a fully implanted version of the BP warning system. Although the first clinical target is AD for persons with SCI, Dr. Kilgore and his team plan to expand the use of this sensor to many other health monitoring applications in the future.
Dr. Kilgore is Professor of Orthopedics, PM&R and Biomedical Engineering, Case Western Reserve University (CWRU). His co-investigators include Pedram Moheseni, PhD, Professor of Electrical Engineering and Computer Science, CWRU; Laleh Najafizadeh, PhD, Associate Professor of Electrical and Computer Engineering, Rutgers University; Greg Nemunaitis, MD, Director of Spinal Cord Medicine, MHS, and Professor of PM&R, CWRU; and Tina Vrabec, PhD, staff scientist, MHS, and Assistant Professor of PM&R,* CWRU.
*Pending CWRU appointment review.
3/11/19 Physical Medicine and Rehabilitation Ranked 2 in NIH Funding
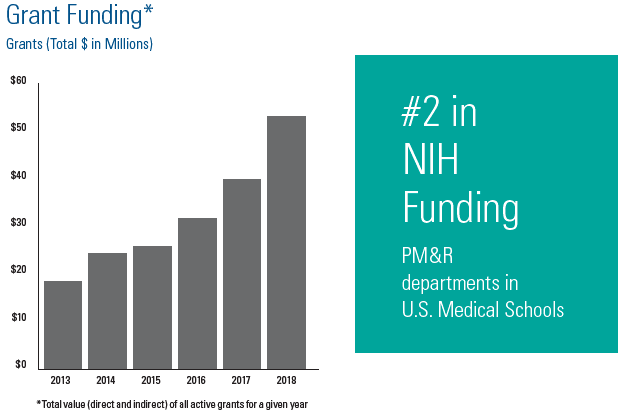 The department of Physical Medicine and Rehabilitation (PM&R) at the MetroHealth System (MHS) and Case Western Reserve University (CWRU) is ranked number 2 in the nation in National Institutes of Health (NIH) funding among PM&R departments in U.S. Medical Schools. The Blue Ridge Institute for Medical Research rankings are based on data released by the NIH for all active awards during the 2018 fiscal year, which began October 1, 2017 and ended September 30, 2018.
The department of Physical Medicine and Rehabilitation (PM&R) at the MetroHealth System (MHS) and Case Western Reserve University (CWRU) is ranked number 2 in the nation in National Institutes of Health (NIH) funding among PM&R departments in U.S. Medical Schools. The Blue Ridge Institute for Medical Research rankings are based on data released by the NIH for all active awards during the 2018 fiscal year, which began October 1, 2017 and ended September 30, 2018.
The department of PM&R at CWRU is based at the MHS and is housed within the MetroHealth Rehabilitation Institute, whose mission is to restore function, societal participation and quality of life for persons with significant neurological and musculoskeletal impairments and functional limitations. The Institute is committed to a transdisciplinary approach that delivers outstanding rehabilitation care, trains the next generation of rehabilitation clinicians and scientists, and discovers new knowledge that translates to clinical practice.
The MetroHealth Rehabilitation Institute is world renowned for the development and clinical implementation of sophisticated electrical stimulation systems that reanimate paralyzed muscles; restore limb, trunk, respiratory, bowel and bladder function; and facilitate neurological recovery following stroke, brain injury and spinal cord injury (SCI). Major new initiatives include interventions for the treatment of chronic pain and cardiac and pulmonary dysfunction in the non-neurologically impaired population. The research program within the Institute is staffed by biomedical engineers, electrical engineers, neuroscientists, neurosurgeons, occupational therapists, orthopedic surgeons, physiatrists, and physical therapists.
The MetroHealth Rehabilitation Institute presently has over $52 million in extramural research funding with two thirds awarded by the NIH. Independent Investigators in the Institute, defined as a Principal Investigator (PI) or Co-PI of a NIH R01 or equivalent award, include:
* Kimberly Anderson, PhD, Professor of PM&R*: Perspectives of people living with SCI and electrical stimulation for motor recovery in SCI (DoD)
* Niloy Bhadra, MD, PhD, Associate Professor of PM&R*: Electrical nerve block (NIH)
* Dennis Bourbeau, PhD, Assistant Professor of PM&R: Electrical stimulation for bladder function in SCI (NIH, VA)
* John Chae, MD, Professor of PM&R & Biomedical Engineering (BME): Peripheral nerve stimulation (PNS) for musculoskeletal pain (NIH)
* Anthony DiMarco, MD, Professor of PM&R & Physiology/Biophysics: Respiratory neuroprosthesis for SCI (NIH)
* Kevin Kilgore, PhD, Professor of Orthopedics, PM&R and BME: Upper limb neuroprosthesis for SCI and electrical nerve block (NIH, VA, FDA)
* Krzysztof Kowalski, PhD, Associate Professor of PM&R*: Respiratory neuroprosthesis in SCI (VA)
* Jayme Knutson, PhD, Associate Professor of PM&R: Electrical stimulation for hemiparesis (NIH, VA)
* Gregory Nemunaitis, MD, Professor of PM&R: SCI Model System (NIDILRR)
* P. Hunter Peckham, PhD, Professor of BME & Orthopedics: Upper limb neuroprosthesis for SCI (NIH)
* Mary Jo Roach, PhD, Associate Professor of PM&R*: SCI Model System (NIDILRR)
* Richard Wilson, MD, Associate Professor of PM&R: PNS for musculoskeletal pain (NIH)
* Pending CWRU review
03/01/19 Kim Anderson, PhD, receives $630,000 Department of Defense Award
Kim Anderson, PhD, a staff scientist in the department of Physical Medicine and Rehabilitation (PM&R), was awarded a $630,000 grant by the Department of Defense (DoD) to lead a clinical trial targeting restoration of reaching and grasping function in individuals with spinal cord injury.
A randomized controlled trial will compare electrical neuromodulation delivered by MyndMove® therapy to intensive upper-limb conventional therapy. The study will enroll individuals with moderate to severe upper limb motor impairment following an incomplete, sub-acute, traumatic spinal cord injury. The trial is sponsored by MyndTec Inc. and funded by the DoD. Dr. Anderson, in collaboration with Dr. James Wilson, will co-lead the trial at the MetroHealth Rehabilitation Institute and Louis Stokes Cleveland Veterans Affairs Medical Center (LSCVAMC), respectively. Other participating centers include Houston, Toronto and Vancouver.
Dr. Anderson joined PM&R in March of 2018 from the University of Miami where she was Professor of Neurological Surgery. Her appointment to Professor of PM&R is pending a Case Western Reserve University (CWRU) review. Dr. James Wilson is a staff physiatrist in the Spinal Cord Injury Medicine service at the LSCVAMC, a staff scientist in the department of PM&R at MetroHealth, and Clinical Instructor of PM&R at CWRU. His appointment to Assistant Professor of PM&R is also pending a CWRU review.
02/11/19 Terry Stancin, MD, receives Joseph D. Matarazzo Award for Distinguished Contributions to Psychology
 The Association of Psychologists in Academic Health Centers honored Terry Stancin, PhD, with the Joseph D. Matarazzo Award for Distinguished Contributions to Psychology in Academic Health Centers. The award is presented by the Association of Psychologists in Academic Health Centers to recognize outstanding psychologists whose work in medical school and health care settings has enhanced the roles of psychologists in education, research, and clinical care.
The Association of Psychologists in Academic Health Centers honored Terry Stancin, PhD, with the Joseph D. Matarazzo Award for Distinguished Contributions to Psychology in Academic Health Centers. The award is presented by the Association of Psychologists in Academic Health Centers to recognize outstanding psychologists whose work in medical school and health care settings has enhanced the roles of psychologists in education, research, and clinical care.
02/05/19 Joan Papp, MD awarded $265,500 grant to expand access to medication assisted treatment in the Cuyahoga County Correction Center
 Joan Papp, MD, Medical Director of the Office of Opioid Safety at the MetroHealth System, was awarded a $265,500 grant as part of the Combatting Opioid Overdose through Community-level Intervention Initiative (COOCLI). The COOCLI is a $3.5 million grant from the Office of National Drug Control Policy managed by the University of Baltimore’s Center for Drug Policy and Enforcement. The subaward from the University of Baltimore will be used to build on the MetroHealth System’s ongoing program in the Cuyahoga County Corrections Center (CCCC) to increase access to medication assisted treatment (MAT) for inmates with opioid use disorder (OUD).
Joan Papp, MD, Medical Director of the Office of Opioid Safety at the MetroHealth System, was awarded a $265,500 grant as part of the Combatting Opioid Overdose through Community-level Intervention Initiative (COOCLI). The COOCLI is a $3.5 million grant from the Office of National Drug Control Policy managed by the University of Baltimore’s Center for Drug Policy and Enforcement. The subaward from the University of Baltimore will be used to build on the MetroHealth System’s ongoing program in the Cuyahoga County Corrections Center (CCCC) to increase access to medication assisted treatment (MAT) for inmates with opioid use disorder (OUD).
Opioid overdose is currently the greatest threat to public health in Northeast Ohio and has been the leading cause of injury death statewide since 2007. Cuyahoga county is among the highest impacted counties statewide with an overdose rate of 28.5/100,000. OUD is prevalent in the incarcerated population who are at a significantly greater risk of fatal opioid overdose upon release. In the CCCC, one third of inmates are diagnosed with OUD and are likely to benefit from harm reduction and treatment interventions.
Dr. Papp and her team will increase access to MAT for inmates with OUD by implementing the following:
1) an expedited process to identify and assess inmates with OUD;
2) an enhanced process to secure an alternative to incarceration program pre-trial;
3) MAT, behavioral treatments and overdose prevention training during incarceration; and
4) an enhanced “warm hand-off” plan connecting the inmate with outpatient OUD treatment and a peer supporter.
The funding will support a forensics coordinator, licensed practical nurse (LPN), a licensed independent social worker (LISW), labs and medications to treat OUD and prevent fatal overdose. Dr. Papp is Assistant Professor of Emergency Medicine and the Case Western Reserve University School of Medicine.
01/10/19 MetroHealth scientists featured for work in electrical stimulation in patients with spinal cord injuries
 The cover of the January 2019 issue of the American Journal of Physical Medicine and Rehabilitation features an article entitled "Complete restoration of respiratory muscle function in three subjects with spinal cord injury."
The cover of the January 2019 issue of the American Journal of Physical Medicine and Rehabilitation features an article entitled "Complete restoration of respiratory muscle function in three subjects with spinal cord injury."
The respiratory neuroprosthesis, developed by MetroHealth scientists Anthony DiMarco, MD and Krzysztof Kowalski, PhD, in collaboration with Robert Geertman, MD, PhD and Kutaiba Tabbaa, MD, provides inspiratory function by electrically pacing the diaphragm and coughing function through electrical stimulation of the spinal cord.
The diaphragm pacing was successful in maintaining three patients off of mechanical ventilation. The coughing system demonstrated peak expiratory airflow and pressures comparable to normal cough. Subjects reported much greater ease in raising secretion with the coughing function, which is critical in reducing the risk of respiratory infections and other pulmonary complications in the spinal cord injured population.
Dr. DiMarco is Professor of Physical Medicine and Rehabilitation; Dr. Kowalski is Clinical Associate Professor of Medicine; Dr. Geertman is Assistant Professor of Neurological Surgery; and Dr. Tabbaa is Clinical Assistant Professor of Anesthesiology, Case Western Reserve University (CWRU) School of Medicine. Dr. DiMarco is the Principal Investigator of the U01 Award from the NIH – National Institute for Neurological Diseases and Stroke that funded the study. The study was also supported by the CWRU Clinical and Translational Sciences Collaborative funded by the NIH – National Center for Advancing Translational Sciences.

01/09/19 Drs. Wilson and Chae Present at Pain Management Workshop
Richard Wilson, MD, Director of the Division of Neurological Rehabilitation in the Department of Physical Medicine and Rehabilitation (PM&R) and John Chae, MD, Chair of PM&R and Vice President for Research and Sponsored Programs, presented at a National Academy of Medicine Workshop entitled “The Role of Nonpharmacological Approaches to Pain Management.”
The workshop, held on December 4-5 in Washington, DC, was based on recommendations regarding nonpharmacological approaches to pain in the 2011 Institute of Medicine report, “Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research” and the 2017 National Academies of Sciences, Engineering and Medicine’s report, “Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use.”
The objective of the workshop was to review the current state of evidence on the effectiveness of nonpharmacological treatments and the use of diverse health models for pain management. Dr. Wilson shared information on implantable devices and nonpharmacological approaches to pain management.
Dr. Chae served on the workshop’s planning committee. Drs. Wilson and Chae are NIH funded investigators with extensive experience in the development and clinical assessment of implantable technologies for the treatment of pain. Dr. Wilson is Associate Professor of PM&R and Dr. Chae is Professor and Chair of PM&R and Professor of Biomedical Engineering at the Case Western Reserve University School of Medicine.
