Bladder & Bowel Function after SCI
Investigators
- Dennis Bourbeau, PhD
- Robert F. Hoey, PhD
- Carvell Nguyen, MD
- James Wilson, DO
Neurogenic bladder and bowel dysfunction are significant challenges for individuals with SCI, resulting in lost independence, lost dignity, social isolation, and medical complications.
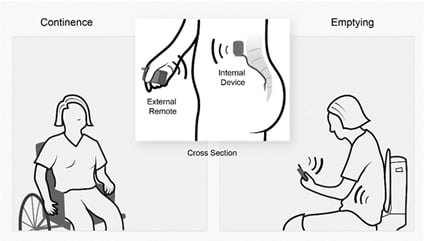
MetroHealth Rehabilitation Institute researchers have been testing approaches using electrical stimulation to improve bladder function by: inhibiting unwanted bladder activity to prevent urinary incontinence, and pursuing electrode implant technologies that seek to improve the ability to empty the bladder by inhibiting unwanted urethral sphincter activity.
 Furthermore, we are presently evaluating the feasibility of closed-loop control of electrical stimulation to relax the bladder and improve urinary continence automatically. This approach uses the pressure signal from a urethral catheter in the human study participant to determine when inhibitory stimulation should be applied to maintain continence and prevent accidents.
Furthermore, we are presently evaluating the feasibility of closed-loop control of electrical stimulation to relax the bladder and improve urinary continence automatically. This approach uses the pressure signal from a urethral catheter in the human study participant to determine when inhibitory stimulation should be applied to maintain continence and prevent accidents.
By using real-time measurements of bladder status, this technology could improve urinary storage capacity and lead to longer time periods between catheterization and therefore facilitate greater quality of life after injury.
Neurogenic changes after SCI include deficits in bowel function that have a significant impact on the quality of life for individuals after SCI. To address these issues we have begun to investigate the effect of peripheral electrical stimulation techniques on bowel function.
We are currently studying the effects of modulating anal sphincter activity and rectal/colonic dynamics using peripheral electrical stimulation. The goal is to reduce fecal incontinence episodes, which are a significant cause of distress and isolation after SCI, with a future goal of aiding in defecation to reduce excessively long bowel program times.
The overriding goal of our group is to use our expertise to develop intervention technologies, for both detection and modulation, to improve the understudied complications of neurogenic bowel and bladder dysfunction.
Moving forward, we will strive to meet this goal by continuing to develop wireless, implantable sensors that can provide continuous data from the bladder or the bowel so that interventions can be applied, as well as refine stimulation techniques to effectively and safely improve function.
For more information about research studies involving Bladder Function after SCI, please contact:
Dennis Bourbeau, PhD
Email: dbourbeau@fescenter.org
or
Kimberly Schach, Coordinator
Phone: 216-778-7992
Email: kschach@metrohealth.org